Veteran HR leader Maria Cartagena shares her decade-long, $200,000 fertility journey, highlighting systemic gaps in medical education and workplace support.
Cartagena advocates for proactive fertility conversations by GPs, including early AMH testing, to empower individuals with timely information.
Workplaces must shift from reactive measures to fostering open, supportive cultures with flexible policies and tangible fertility benefits.
A seasoned HR executive with a track record of scaling tech companies through rapid growth and successful exits, Maria Cartagena brings a wealth of experience in building people-centric organizations. But it's her deeply personal, over-a-decade-long fertility journey—spanning six clinics in three countries—that has ignited a passion to transform how society and workplaces approach fertility.
"I am now $200,000 into fertility treatment," Cartagena says, a massive figure that is unfortunately not an outlier. Her journey began later in life after meeting her partner, and quickly revealed unexpected realities about infertility.
Rising rates: "I am the oldest person at every clinic I have been to," Cartagena shares. "The most stunning realization I had through this process was that infertility isn't just for folks like me who waited a little bit longer." This observation, she notes, points to a broader, often unacknowledged, issue of rising infertility rates among younger populations.
The financial reality is just as stark: "I could have frozen my eggs in my 20s for $10,000-12,000 and given myself more windows for treatment options over time, but nobody was talking to me about it at the time."
A call for proactive intervention: The lack of early information is a critical failure point Cartagena aims to address in her new advisory role at myStoria. "The conversation with your doctor needs to change," she urges. "The fact that they do all this blood work as a standard as part of your physical, along with your blood work for blood sugar and cholesterol is a good starting point, but they should add AMH on that list."
She emphasizes the relatively low cost of an Anti-Müllerian Hormone test, which indicates ovarian reserve is relatively affordable in Canada and the U.S. Yet, many general practitioners "didn't even know what AMH testing was." The delay in crucial information can be devastating. "[Waiting for a referral] could literally cost a lot more time. Once you hit 43 years old, most clinics won't do IVF anymore. If you're waiting until you're 40 to start the process, and it takes time to get into a clinic, you're getting closer to that number, in which case almost all your windows for treatment are closing."
Transforming the workplace narrative: Cartagena’s HR background, including her role as Chief People Officer at Kira Systems, provided a platform to implement change. "Acting like family planning is not something that happens to most people in the workplace needs to stop," she asserts. "This is a natural part of life."
At Kira Systems, which was "flexible first before COVID ever happened," the approach was foundational. When interviewing, she was open about her fertility journey. The reponse from the founders Alexander Hudek and Noah Waisberg—"We hope it works, and when it does, we'll figure it out"—solidified her decision. "I knew at that point they felt the same way that I did. I will build processes, I will build a team, I will build all the policies and programs in place so that if I do successfully get pregnant and go off, the company will still keep running."
But that trust is often missing. So Cartagena implemented parental leave policies, $4,000 in fertility benefits ("it was not a prohibitively expensive add!"), and fostered a culture of open conversation. "I openly talked about fertility at the company so that it sent a signal to others that this was a safe space to talk family planning."
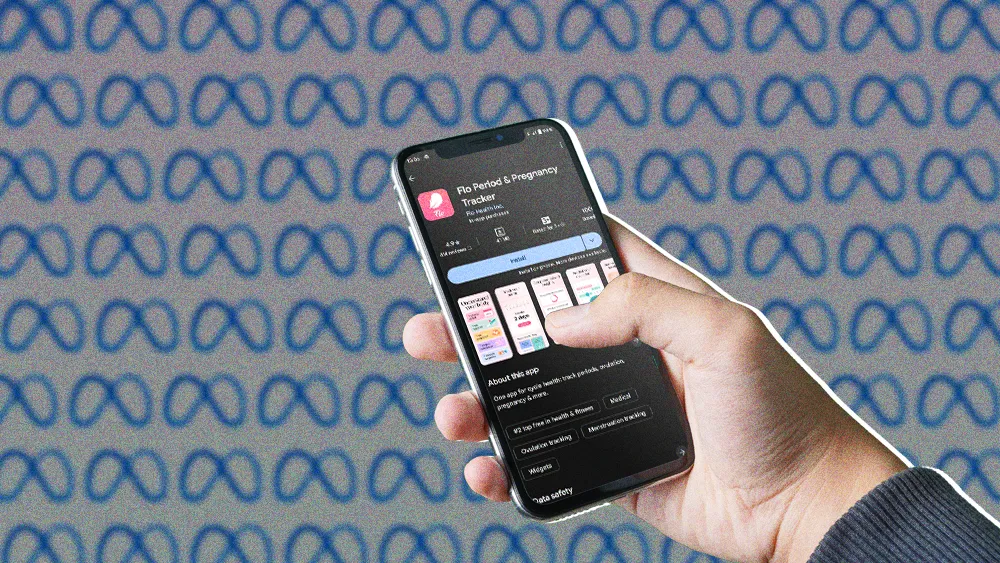
The power of "Big Sister Medicine" and myStoria: "Navigating the complexities of fertility treatment often feels like 'crowdsourcing medicine', which is unbelievable in this day and age," Cartagena says. This is where "Big Sister Medicine"—individuals sharing experiences and guidance—and platforms like myStoria become vital.
The next wave of essential benefits: Cartagena believes that comprehensive fertility and family planning support is no longer a niche perk, but an essential component of employee wellbeing. "Employers may make the mistake of thinking it's probably 1 or 2% of their population that's going to use the support. But the reality is, they have no idea how many people are actually going through this at work because they're not talking about it openly."
Creating a culture of support, she argues, costs nothing initially. From there, companies can build out benefits and policies. "If you're going to use parental leave, try to make it fair for everyone, despite what their role is in the pregnancy journey."
A steadfast mission: Despite her advocacy and the support she's championed for others, Cartagena's personal journey continues. "To date we are a decade in and we still don't have a baby," she shares candidly. "65% of people [for whom IVF doesn't work] walk away. We're on to donor eggs now. I may have to go to surrogacy, which is potentially another 5- to 6-figure financial decision, along with the emotion of losing the ability to carry." The raw honesty underscores the profound emotional and financial stakes involved, and the resilience required. Her experience fuels her mission: to ensure others have the information, support, and workplace understanding she often had to fight for.